In Short
- Healthcare businesses must follow strict privacy and data security rules when handling patient information.
- Prescriptions can only be issued by authorised professionals following a thorough patient assessment.
- Healthcare professionals must meet high standards of care, honesty, and patient safety in their practice.
Tips for Businesses
To ensure compliance, healthcare businesses should establish clear protocols for data privacy and secure patient information handling. Additionally, ensure that all prescribing and care decisions are made by authorised professionals following legal guidelines. Regularly review compliance with healthcare laws to avoid legal issues.
Understanding and managing the complex legal compliance frameworks in the healthcare industry can feel overwhelming. This article will take you through three critical legal frameworks that are essential to be aware of for any healthcare business and healthcare practitioners. It will also look at privacy and data security regulation, regulation of prescription, and how the law governs how healthcare professionals conduct themselves.
Privacy and Data Security
Most healthcare businesses will deal with personal or confidential information in some form. Handling patients and managing their medical records will place your business or you as a practitioner in possession of information that, by law, receives specific protections.
Patient Privacy
Healthcare entities must follow the law when collecting personal information. You should collect patient information directly from the patient unless it is impractical or unreasonable to do so. You may collect information without the patient’s consent if it is necessary to prevent a serious threat to an individual’s life, health, or safety or to public health and safety. However, you must not collect information through intimidation, deception, or in an overly intrusive way.
When you collect personal information, you must inform the patient of the purpose and provide details, such as:
- your organisation’s contact information;
- how patients can access their data; and
- whether the collection is authorised by law.
Patients can request anonymity, meaning they exclude their personal identifying details. However, you do not need to deal with patients anonymously if it is impractical or authorised by law.
Using and Disclosing Personal Information
You may only use and disclose personal information for the primary purpose for which the organisation collected it, and only if the patient reasonably expects that the organisation will do this.
You can only disclose it for another purpose with the patient’s consent unless you reasonably believe that doing so would reduce a serious threat to someone’s life, health, or safety, or public health or safety.
Giving Access
Patients have the right to request access to personal information that they have provided you with. They can access anything from a single piece of information to an entire medical record. You must grant them access to the information within a reasonable timeline unless you believe that providing them with access will worsen a serious threat to the life, health and safety of any individual, or to public health or safety, or that access will endanger the privacy of some other patient, or some other reason permitted by law.
Prescribing Medicines
A prescription is a legal document. Obtaining medicines that are required by prescription is illegal without the relevant prescription. Before making a prescription for a patient, a doctor must:
- ensure that they have adequately assessed the patients’ circumstances and symptoms;
- consider other medicines that the patient is taking to prevent any adverse interactions; and
- explain the potential side effects and risks associated with taking the medicine.
Practice
The law requires that doctors follow specific standards of conduct and care. Industry codes of conduct prescribe particular characteristics and behaviours that a doctor requires. Some of these characteristics and behaviours include the following:
- a doctor must make the care of their patients their first concern;
- a doctor must be honest, ethical and trustworthy;
- doctors must practise medicine safely and effectively;
- doctors should practise in a manner that is culturally safe and respectful;
- decisions about a patient’s access to medical care must be free from bias and discrimination;
- a doctor must maintain a high level of medical competence and professional conduct;
- doctors must be effective communicators;
- doctors must properly inform patients when attempting to obtain consent;
- a doctor must be alert to whether children and young people in their care are at risk and inform the relevant authorities;
- doctors must acknowledge and do their part to manage risk;
- doctors must observe and maintain professional boundaries with their patients; and
- doctors must resolve conflicts of interest in the best interest of the patient.
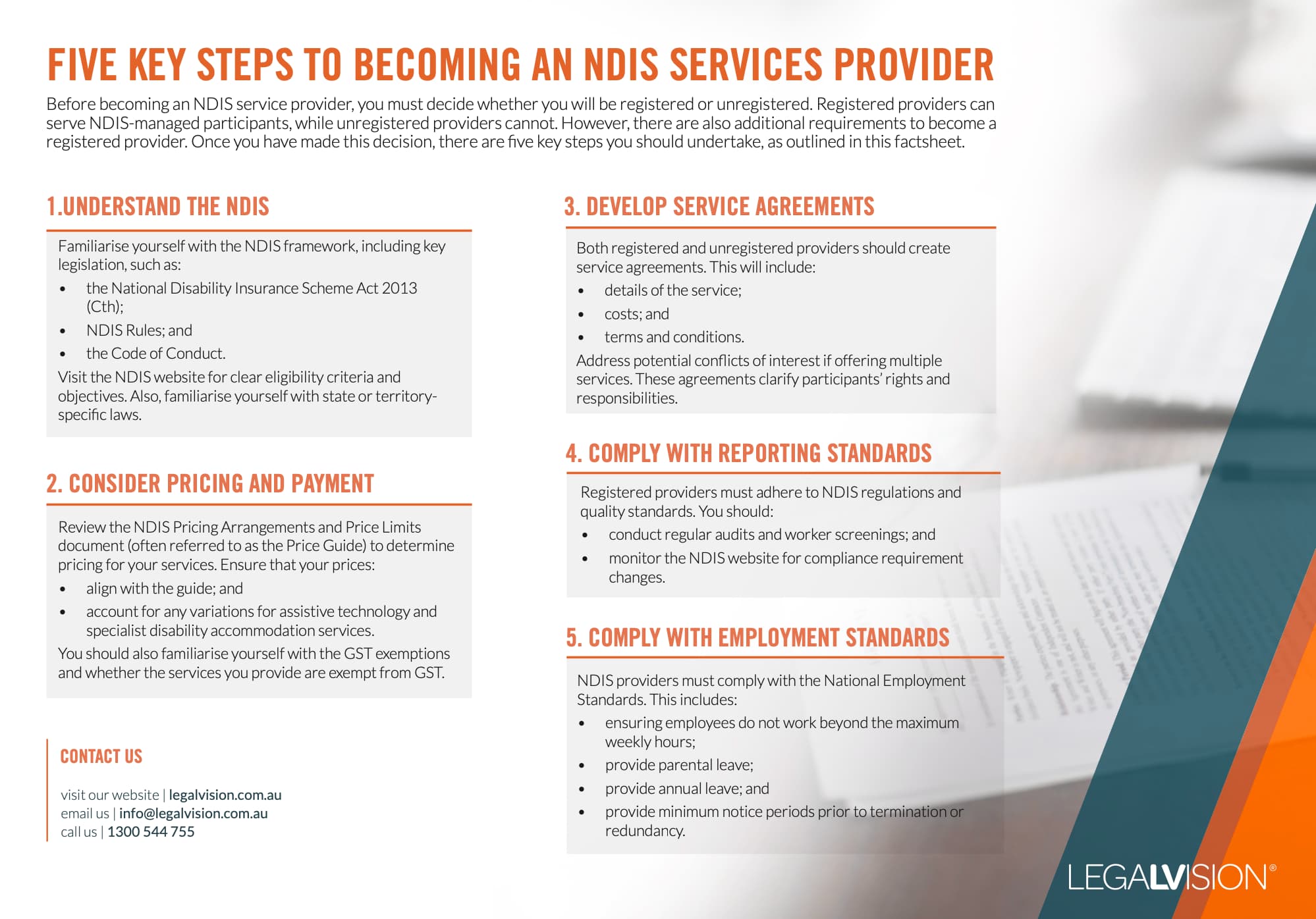
Understand five key steps you should know to become an NDIS service provider with this free LegalVision factsheet.
Key Takeaways
When practising as a medical professional or managing a healthcare business, medical professionals and healthcare managers must consider three essential legal frameworks. They include:
- The privacy and patient personal information protection regime ensures that medical practitioners only collect, use, or disclose information when authorised by law. Information should only be used or disclosed for the purpose it was collected. Patients have the right to access their personal information.
- Prescriptions can only be made by authorised professionals and should be made after a close assessment of the patient’s circumstances.
- Codes of conduct require doctors to comply with specific standards of behaviour, including practising safely and effectively, maintaining professional boundaries and making decisions without bias or discrimination.
If you need help navigating the compliance frameworks in the healthcare space, our experienced healthcare lawyers can assist as part of our LegalVision membership. For a low monthly fee, you will have unlimited access to lawyers to answer your questions and draft and review your documents. Call us today on 1300 544 755 or visit our membership page.
Frequently Asked Questions
Healthcare professionals must collect patient information directly unless impractical. They can only use or disclose personal information for its intended purpose and must inform patients how their data will be used. Patients have the right to access their information promptly.
Only authorised health professionals, like doctors and nurse practitioners, can prescribe medication. Before prescribing, they must assess the patient’s circumstances, consider possible interactions with other medications, and explain any risks and side effects.
We appreciate your feedback – your submission has been successfully received.











